[Product Promotion] TMB Diagnostic Standard
Tumor mutation burden (TMB) refers to the number of somatic mutations in the tumor genome after germline mutations have been removed. It is defined as the total number of somatic gene coding errors, base substitutions, gene insertion or deletion errors detected per million bases. Tumor mutation burden is a quantitative biomarker, which reflects the total number of mutations carried by tumor cells. Tumor cells with high TMB have higher levels of neoantigens, which are thought to help the immune system recognize tumors and stimulate the proliferation of anti-tumor T cells and anti-tumor responses. Mutations in tumor cells will accumulate over time, which is not seen in normal cells.
The current detection methods on the market refer to the number of somatic mutations per million bases (Mb) of the coding region of the patient's targeted sequencing, including point mutations and indels. The number of somatic mutations in different cancers ranges from 0.01 mutation/Mb to over 400 mutations/Mb.
The higher the tumor mutation burden, the more tumor-related carcinogenic mutations, the more prominent the tumor’s personality and the more different from normal cells. The more mutated genes in tumor tissues, the more likely it is that new antigens (or new epitopes), protein fragments/peptides, etc. produced are recognized as non-self antigens by the immune system, and the more likely it is to activate T cells by the immune system See through, thereby activating the body's anti-cancer immune response, the better the efficacy of receiving immune checkpoint inhibitor treatment may be. That is, the higher the TMB, the better the effect of tumor immunotherapy.
At present, there is more and more evidence to support tumor mutational burden (TMB) as a potential predictor of efficacy. The clinical research data of multiple tumor types show that in the PD-L1 unselected population or the PD-L1 positive population, the higher the mutation load, the efficacy of PD-1/PD-L1 inhibitor treatment is positively correlated with TMB. TMB has good predictive value for immunotherapy of various tumors. The predictive effect of TMB is better than PD-L1 expression.
In June 2020, tumor mutation burden TMB was approved by the FDA for companion diagnostics, and unresectable or metastatic tumor tissue samples with high mutation burden (TMB-H) ≥10 mutations/Mb were approved for adult and child solid tumor patients (previous After treatment, the disease progresses and there is no better alternative therapy), pembrolizumab can be used as a single agent. This makes TMB the second pan-cancer species companion diagnostic marker for tumor immunotherapy after MSI/dMMR, and also the third pan-cancer species marker that does not need to consider the source of tumor organs.
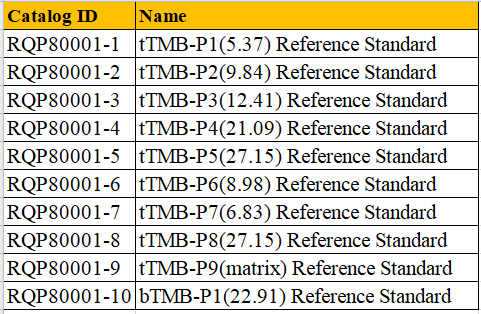
We can provide TMB diagnostic standards to ensure the detection limit, sensitivity and stability of the diagnostic method.